Implementation
Program implementation is defined as a specified set of activities developed to put strategies of the program into practice. Based on the program or intervention goals and objectives, an implementation plan (See Section 1.3) should be developed to provide a detailed framework for the activities, including what the activity is, who is responsible for the activity, and what the timeline is to achieve the objectives.
For a program whose goal is to increase access to high-quality contraceptive services, program implementation should focus on activities specific to contraceptive service delivery. This Section addresses basic components of program implementation.
Service delivery is providing a specific set of health care services to patients to meet their health needs and expectations. In a program to increase contraception access, the delivery of high-quality contraceptive services includes screening women for pregnancy intention; providing women with client-centered contraceptive counseling; using evidence-based guidelines to initiate contraception and manage side effects; and ensuring the patient’s choice in method selection, discontinuation, and method switching. The development of service delivery strategies ideally includes careful assessment of any intentional or unintentional barriers that may block women’s access to services and removal of these barriers in accordance with evidence. It also is important to assess the quality of service delivery from the perspective of women who have received services and to compare this information with the data reported by providers at the time of service delivery.
Key components of service delivery:
- Building capacity among providers, staff, and clinic administrators (See Sections 2.1, 2.3, 2.4)
- Assessment of overall clinic readiness (See Section 2.4)
- Procurement, distribution, stocking of methods within clinics (See Section 2.5)
- Development of a process for booking appointments for this new service (if advanced bookings are the norm in the context of service delivery)
Components of service delivery:
- Intake: A front desk or administrative person, support staff, or nurse may be responsible for intake. Ideally, all staff involved in contraception service delivery are well informed on service processes and procedures such as data collection forms, available methods, and cost sharing.
- Client-centered contraception counseling: Job aids (patient information
tools used by providers) or visual aids are often used and can be helpful during
counseling. Supporting patient preference and autonomous decision-making is critical
- Assessment of eligibility for method of choice and for initiation of method on the same day of the visit (Quick start).
- Initiation of methods:
- Patients receive information on the selected contraception method that include instructions for use, management of side effects, awareness of danger signs, and a six-month supply of short-acting method (pills, patch, ring), or initiation of progestin injection with a follow-up appointment in approximately three months
- Patients who select a long-acting reversible contraception (LARC) method (intrauterine device [IUD] or implant) receive the insertion of the chosen LARC method, discussion of potential side effects and management strategies, awareness of danger signs, and instructions for follow up.
- Return visits: These visits may occur as planned visits or visits made due to side effects, questions or concerns, desire to discontinue or remove a method, or to switch methods. It is important during all visits, including return visits, to ensure patients receive client-centered counseling and that providers respect patients’ autonomous decision-making.
- Documentation:
- Ideally, all data collection and clinic visit forms use standardized indicators that are tied to the particular program.
- Different contexts or settings may add other indicators, depending on the situation (pandemic, natural disaster, conflict, preparedness, stable setting).
Lessons Learned:
- Prepare for changes that may occur in the clinic flow with the addition of contraceptive services.
- Anticipate staff and provider time needed to adapt to this new component of service delivery. This will likely diminish over time, but the time commitment per patient may be substantial at service delivery start-up sustain high quality.
- Anticipate demand for the new service in the catchment area served by the clinic or health center site.
- Adjust the number of providers available and clinic templates accordingly.
- Consider ways to manage patient expectations for clinic wait time and the wait time for a first appointment. Determine the acceptable range in your context (one day, one week, or one month?).
- Clarify with patients any expectations for cost sharing for services, methods, return visits, or management of any complications.
- Consider role-plays of clinic flow run-throughs before service delivery starts. This will help individual sites assess their own readiness to begin services.
RESOURCES AVAILABLE:
- 3.1a U.S. Medical Eligibility Chart English
- 3.1b U.S. Medical Eligibility Criteria 2016
- 3.1c Providing Quality Family Planning Services - Main Document
- 3.1d Providing Quality Family Planning Services - Update
- 3.1e U.S. Selected Practice Recommendation 2016
- 3.1f U.S. Selected Practice Recommendation SPR Chart - When to Start
- 3.1g Examinations and Tests Needed Before Initiation of Contraceptive Methods
- 3.1h Recommended Actions After Late or Missed Combined Oral Contraceptives
- 3.1i Management of Women with Bleeding Irregularities While Using Contraception
Collecting data to monitor program activities and evaluate your program’s impact is a key component of program implementation. There are various methods for collecting patient encounter data, and the best method for your program will depend on many factors as described in Section 2.6. When thinking about the types of data to collect for your program, consider your program needs, who will be collecting the data, and how the data will be used.
Z-CAN Example: Uses for Patient-Encounter Data
Z-CAN Program staff monitored patient-level data by demographics, visit type (initial visit encounter, return visit encounter, and adverse event), and contraceptive method selected
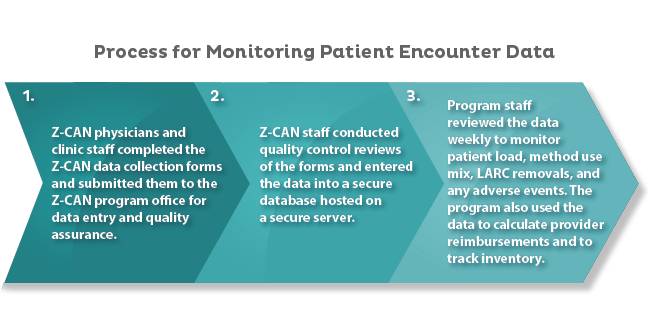
Process for Monitoring Patient Encounter Data
- Z-CAN physicians and clinic staff completed the Z-CAN data collection forms and submitted them to the Z-CAN program office for data entry and quality assurance.
- Z-CAN staff conducted quality control reviews of the forms and entered the data into a secure database hosted on a secure server.
- Program staff reviewed the data weekly to monitor patient load, method use mix, LARC removals, and any adverse events. The program also used the data to calculate provider reimbursement and to track inventory.
Lessons Learned:
- Minimizing changes to the data collection forms allows the providers and clinic staff to operate efficiently and makes data management easier.
- Changes should only be made if necessary to correct misinterpretations of the data collection forms or to capture data for new issues that come up during the course of the program.
RESOURCE AVAILABLE:
Your program or intervention should establish policies and procedures that define which components of the program are offered at no cost to the patient; which services patients will be expected to pay for; and which services providers will be paid to do, either directly by the program or through an insurance billing or reimbursement system. Program staff must be well versed in these policies and procedures, so they can provide an explanation of anticipated cost to patients before any visit. This explanation should describe services offered and any charges that might be incurred, if the patient qualifies for a sliding fee scale (if applicable), if an insurance program will be billed, or if there will be any out-of-pocket costs. Clinic staff should be able to answer patient questions and effectively communicate the reason for any out-of-pocket costs.
Z-CAN Example: Policies, Procedures, and Communication about Z-CAN Costs
The Z-CAN program provided women same-day access to contraceptive services at no cost. Policies and procedures developed for Z-CAN physicians and clinics included clear language defining what contraceptive services the Z-CAN program covered and did not cover. Example scenarios were provided to Z-CAN clinic staff to help them understand how to apply the charge policies to patient scenarios. These examples of Z-CAN policies and procedures can be adapted for your program.
RESOURCES AVAILABLE:
Successful implementation of your program requires that providers and clinic staff have access to all of the equipment and supplies necessary to provide services. Whether these are provided by the program or are minimum requirements for participation in the program will depend on the program’s budget and the general availability of the items for standard services.
Consider cost and logistics when deciding on provision of equipment and supplies:
- Does the program budget support provision of the equipment and supplies that will be needed, including shipping costs? If not, does the budget support provision of critical items needed or items that may be difficult to obtain?
- Are the equipment and supplies needed for the program already standard for a typical clinical practice?
- Are the barriers to obtaining the necessary equipment and supplies?
Lessons Learned: Resources for Supplies
Equipment and supplies for securely storing contraceptive products, insertion of LARC methods, and collecting, submitting, and storing Z-CAN program data were requirements of the Z-CAN program. The availability of the required equipment and supplies was assessed in each clinic during the clinic mentoring visit (See Section 2.4). While the equipment and supplies needed were typical of an obstetrics and gynecology (ob-gyn) practice, the Z-CAN program identified five key items that could be provided by the Z-CAN program to clinics if needed (uterine sound, tenaculum, ring forceps, os finder, and refrigerator).
Lessons Learned: Resources for Supplies
- If your program budget does not allow for provision of key equipment and supplies needed to provide services, having a contact list of resources available for obtaining the items would help ensure that providers and clinic staff are able to comply with program requirements to provide high-quality services.